Concordant peripheral lipidome signatures in two large clinical studies of Alzheimer’s disease
Photo by metamorworks/iStock / Getty Images
Huynh K, Lim WLF, Giles C, Jayawardana KS, Salim A, Mellett NA, Smith AAT, Olshansky G, Drew BG, Chatterjee P, Martins I, Laws SM, Bush AI, Rowe CC, Willemagne VL, Ames D, Masters CL, Arnold M, Nho K, Saykin AJ, Bailie R, Han X, Kaddurah-Daouk R, Martins RN, and Meikle PJ. Concordant peripheral lipidome signatures in two large clinical studies in Alzheimer’s disease. Nature Communications, 11
Alzheimer’s disease researchers have been searching for biomarkers to be used for early detection of the neurodegenerative disease for decades. This work requires large well-designed clinical studies. There are two leading cohort studies that have been designed to support the identification of biomarkers associated with Alzheimer’s disease (AD) and employing this knowledge to take a proactive approach to mild cognitive impairment (MCI) and AD diagnoses through early detection. The Australian Imaging Biomarkers and Lifestyle (AIBL) is a large longitudinal study consisting of over 1000 patients in Australia with the goal of identifying biomarkers, lifestyle variables, and cognition levels associated with the onset of AD. Similarly, the Alzheimer’s Disease Neuroimaging Initiative (ADNI) is a longitudinal cohort study based in North America which has enrolled over 1500 participants. The focus of ADNI is to identify AD markers, with a strong focus on imaging, and further to evaluate the brain changes leading to AD and its progression. AD is a neurodegenerative disease consisting of memory loss and cognitive decline that affects 500 000 Canadians with the incidence expecting to double by 2035 (1), and 81 million worldwide by 2040 (2). The cause behind AD has not been elucidated, but a number of factors are thought to increase risk, including the accumulation of toxic proteins, improper cholesterol transport, diet and exercise level, and history of mental illness. Huynh et al studied 5733 samples from 1912 participants of the two cohorts using liquid chromatography-mass spectrometry (LC-MS) to analyze the relationship between over 500 species of lipids and AD.
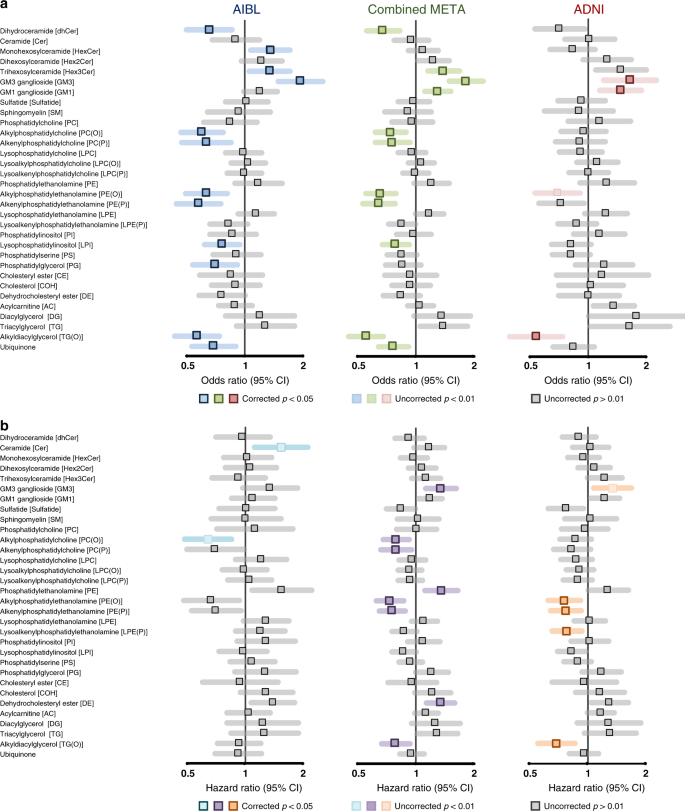
After correcting for factors including age, sex, cholesterol, site of collection, and body mass index, 147 and 87 lipids were found to be associated with AD from AIBL and ADNI, respectively, in both prevalent (Panel A) and incident (Panel B) AD. The importance in this distinction is that it considers both the total number of cases in the population (prevalence), as well as focusing on new cases over a period of time (incidence) to determine the biomarkers of AD. The lipid classes found most closely correlated to AD were sphingolipids and ether lipids. Overall, the ether lipid species, including plasmalogens containing the vinyl-ether bond, were found to be negatively associated with AD. This effect was heightened when the lipids contained omega-3 fatty acids, including docosahexaenoic acid (DHA). These results support previous studies which have shown reduced levels of plasmalogens correlate with the onset and severity of AD. The vinyl-ether bond at the sn-1 position of plasmalogens allows the two fatty acids to have a more compact structure impacting membrane structure, organization, and function and affecting neurotransmission and vesicular fusion.
This independent study by Huynh et al is one of the most comprehensive and well-characterized lipidomic analyses for the biomarkers of AD. Their finding of the negative correlation between ether lipid levels, including plasmalogens, and disease provides strong support for the critical role of these lipids in the disease course. The authors hypothesize that the reduction in all classes of ethers supports a biosynthetic defect and malfunctioning peroxisomal activity which would reduce the production of all ethers. While this has been suggested in the past, others have suggested that reductions in plasmalogen levels is due to oxidation of the vinyl-ether bond in the presence of increased oxidative stress. This study provides strong supports for the hypothesis that plasmalogens are key drivers in Alzheimer’s disease process and validates our goal of developing plasmalogen-based diagnostic and therapeutic products for the identification and treatment of individuals with AD.
1) Alzheimer’s Society of Canada. (2016) Dementia numbers in Canada. https://alzheimer.ca/en/Home/About-dementia/What-is-dementia/Dementia-numbers
2) Ferri CP et al (2005) Global prevalence of dementia: a Delphi consensus study. Lancet 366, 2112–2117.
Fig. 2 Associations of lipid class totals with prevalent and incident Alzheimer’s disease. Forest plots of lipid class associations for a prevalent Alzheimer’s disease (logistic regression, AIBL = 268 cases, 696 control, ADNI= 178 cases, 210 controls) and b incident Alzheimer’s disease (Cox regression, AIBL = 68 cases, 714 controls, ADNI= 166 cases, 397 controls). Lipid classes are generated by the sum of each individual species measured in each class. Regressions are adjusted for age, sex, BMI, total cholesterol, HDL-C, triglycerides, number of APOE4 alleles, statin use and omega-3 supplementation. AIBL was further adjusted for time points (only in logistic regression analysis) and site of blood collection. ADNI was further adjusted for fasting status.